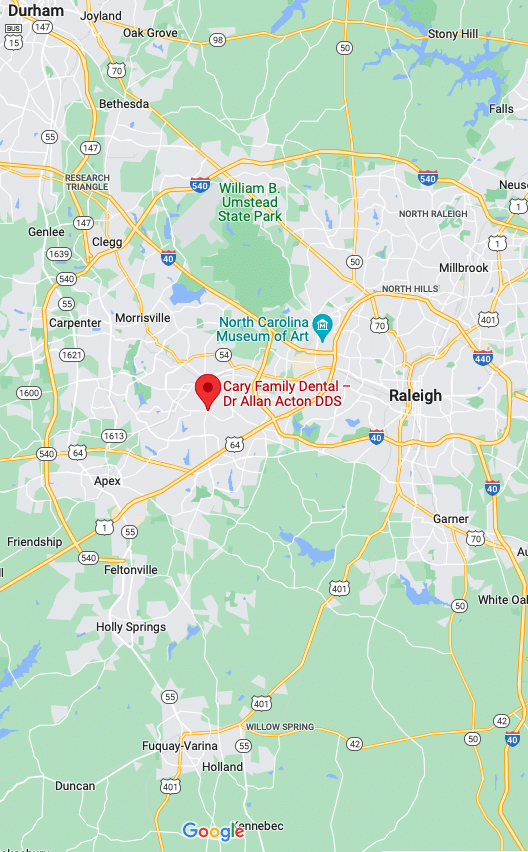
As a courtesy to you, our team will help you know your insurance benefits as well as various payment and financing options available to you. We have many patients that use insurance as a way to assist them with getting their dental needs covered. While we are not in network with any insurance providers, we do accept and file all PPO claims as a courtesy, but are not currently under DMO/HMO plans. All plans are different as it is based on how your employer purchased the plan from the insurance company.
We would be happy to complete a complimentary benefit check so that you can better understand your coverage. Feel free to call the office directly or use our online chat button and one of team members will be happy to assist you.


Understanding Co-Payments
Although most insurance plans allow 2 cleanings per year at 100% coverage, they are covered at 100% of their “allowed amount.” An allowed amount is the average amount an insurance company will pay for any services in a certain geographical area. Most times your co-pay will be $20 or less. Some plans will apply your deductible to preventive services. Each time you have a hygiene appointment or an emergency visit with the doctor there is a strong possibility that an examination will be completed and charged. Most insurance companies will allow 2 exams per year no matter the type of exam. Please be mindful of this and how your insurance policy is written. We will do our best to provide you with the most up-to-date information.
Collecting Insurance Information
If you forget to bring your insurance information to your appointment, there are a few ways we can proceed with your appointment: (1) Give us your employer and we might already have that information in the system. All we will need is your SS# or insurance ID number. (2) Call your HR person and have them give you the name of the insurance company, group number and the insurance company’s contact information and we can most likely take it from there. (3) Pay in full for your services and receive a courtesy (savings from 3 to 5 %) and we will file the claim for you so you may be reimbursed directly.

Frequently Asked Questions
We know understanding your dental insurance benefits may be difficult. While every plan is different, these are some of the most frequently asked questions that can help you better understand your plan.
Why aren’t all of my treatment costs covered?
Dental insurance works differently than typical health insurance. Dental insurance is a money benefit applied by an employer to help the employee pay for routine dental treatment. While the plan is based on the amount of the monthly premium cost, most plans are designed to only cover a portion of the total cost.
What if my plan says it covers 100% of exams and certain other procedures?
Insurance carriers allow a certain dollar amount and will agree to apply 100% of that allowed amount to certain procedures. However, if your dental treatment costs more than the allowed amount, there may still be a balance leftover. The best resource in understanding your unique insurance plan is your Employee Benefits Coordinator or Human Resource department where you work.
How does my insurance carrier come up with its allowed payments?
Often you will see allowed payments referred to as UCR payments (usual, customary and reasonable). These are negotiated amounts between the insurance company and your employer based on where you are located and the premium cost your employer is willing to pay. Usual and customary amounts are typically much less than what dentists in your area will charge for a dental procedure. It does not mean that the dentist is charging an unfair rate.
Will there always be a balance left for me to pay?
Most negotiated allowed payments will only cover a portion of your treatment. Even if the treatment is not covered in full, most people benefit from reduced costs after insurance in applied.
Why is there an annual maximum on my benefits?
Annual dental maximums are the limit that an insurance carrier has agreed to cover for you each year. These limits have not changed since the 1960s.
Why does my benefit plan require me to elect a dentist from a list?
Typically, dentists that appear on an insurance carriers list are those who have agreed to a contract with the benefit plan. These dentists are held to certain restrictions and requirements. There is nothing wrong with dentist who do not appear on the list. Some are not comfortable with these restrictions on treatment.
Why does my plan only pay for the least expensive alternative treatment?
Your dentist will recommend the very best treatment option for your needs; however, the insurance plan may only allow coverage for the least expensive treatment method. This is one way a dental plan works to save money.
Why are X-rays, cleanings and gum treatment not covered?
Insurance plans have specific amounts of certain treatments that it will allow for annually. Often x-rays, cleanings, and gum treatments are among those because they are frequently needed.
Why can’t I get treatment done and send in the claim the next month so that insurance will cover it?
State laws regulate dentists from changing the date of service on a claim to accommodate when the insurance plan officially goes into effect.
What should I do if my treatment is covered and I think it should be?
Unfortunately, dentists have no power to make the insurance company pay because the coverage is an agreement between the patient, employer and the insurance company. The best way to contest a claim is to address it with your Employee Benefits Coordinator at your place of work or directly with the insurance carrier.
What Our Patients Are Saying!